Hearing Aid Insurance Benefits












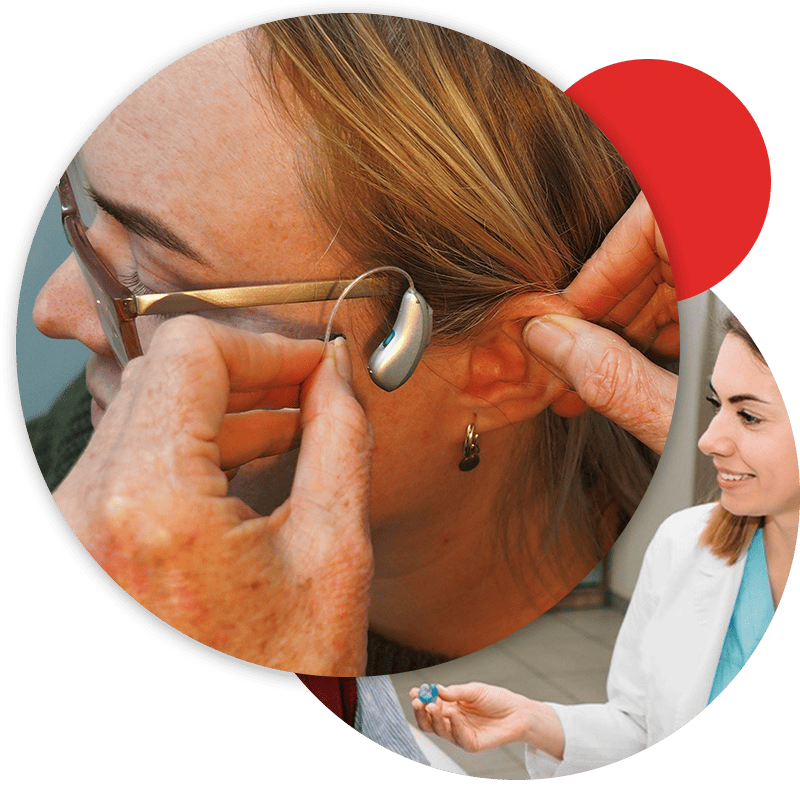
At American Hearing + Audiology, our mission is to provide our patients with the best care possible.
The friendly specialists at our 19 hearing center locations in Kansas City, Lincoln, Tulsa, Arkansas, Tennessee, and Omaha are ready to help you verify your insurance coverage and maximize your savings.
If you’d like to learn more about your insurance benefits for hearing aids, contact your nearest hearing center today.


What Is Hearing Aid Insurance?
Insurance companies offer coverage for hearing aid costs. Plans may cover hearing aid purchases and fittings fully or partially. They might also include a few maintenance visits for cleanings and repairs. Coverage varies by plan, so check your policy’s details before buying hearing aids. Our specialists will assist you at every step.
At American Hearing + Audiology, we aim to maximize your hearing aid insurance benefits. Our experts will explain your coverage details and associated costs. We commit to helping you use your insurance effectively for the greatest advantage.
Vast In-Network Hearing Aid Benefits


Peace of Mind
We understand the challenges of hearing problems, both physically and emotionally. We’ve partnered with a wide network of insurance providers to accept all major plans. This ensures American Hearing + Audiology covers your hearing aid needs.
Our team is ready to assist you in accessing the necessary hearing health care, anytime, anywhere. Don’t wait—contact American Hearing + Audiology today. Discover why we’re the top in-network hearing aid provider in Kansas City, Lincoln, Omaha, and Tulsa. We’re eager to offer you the best hearing aid care and maximize your insurance benefits with our services.
Our Providers
At American Hearing + Audiology, we are devoted to helping you live your best life with improved hearing. Our team of seasoned professionals has a collective 250 years of experience in the field. We guarantee you’ll receive only the highest level of care and attention. Our 19 centers across Kansas City, Lincoln, Omaha, & Tulsa offer private practice settings. Our local audiologists and hearing specialists aim to help you live life more fully.
Does insurance cover hearing aids?
Insurance coverage for hearing aids varies depending on the insurance plan and the specific policy. Fortunately, we’re in-network with all major insurance carriers to maximize your savings with in-network hearing care. If you’re unsure, our expert staff will gladly help verify your hearing aid insurance benefits. Give us a call today!
What is the difference between in-network and out-of-network hearing aid provider?
In most cases, an in-network hearing aid provider will offer a greater discount on services than an out-of-network provider. We are the largest in-network hearing aid provider in the Kansas City, Lincoln, Tulsa, and Omaha areas.
- AARP
- Aetna
- Blue Cross Blue Shield
- Cigna
- Humana
- TriCare
- United Healthcare
- Medicare Advantage
- Nations Hearing
- TruHearing
- UnitedHealthcare Hearing
How do I find out if my insurance covers hearing aids?
The best way to find out if your insurance policy covers hearing aids is to contact your nearest American Hearing & Audiology location! Our insurance specialists will work with your insurance to verify your hearing aid benefits. Since we’re in-network providers for all major insurers, we’re often able to help patients get premium hearing aids for little to no out-of-pocket cost. That’s right, we make it easy to get the most from your hearing aid insurance benefits.
Is my deductible going to be affected by this process of getting hearing aids?
Yes, the cost of hearing aids will likely be applied toward your deductible, depending on your insurance plan. This means that the amount you pay for the hearing aids may count towards your annual deductible, which is the amount you’re required to pay before insurance starts covering a portion of your healthcare costs. However, our team can help you fully understand your insurance coverage and deductible requirements, as well as any potential out-of-pocket costs associated with the process of getting hearing aids through American Hearing.
Why should you visit a hearing care provider that's in-network?
It is important for your hearing care provider to be in-network because it can help you save money on the cost of your hearing healthcare services. When an audiologist is in-network with your insurance provider, they agree to accept the insurance company’s negotiated rates for their services. This means that you will typically pay less out-of-pocket for your appointments, tests, and any hearing aids or accessories that you may need.
Here are a few specific reasons why it’s important to choose an in-network hearing specialist and audiologist:
- Lower costs: In-network audiologists have agreed to accept lower rates for their services in exchange for being included in the insurance company’s network. This means that you will typically pay less for your appointments and any other hearing healthcare services that you receive.
- More affordable hearing aids: When you visit an in-network audiologist, your insurance plan is more likely to cover a higher percentage of the cost of your care. This means that you will have more coverage and may be responsible for less of the cost.
- Fewer surprises: When you visit an in-network audiologist, you are less likely to be surprised by unexpected costs or denied claims. In-network providers are required to follow certain rules and regulations set by the insurance company, so you can have more confidence that your costs and coverage will be consistent with what you expect.
Overall, choosing an in-network audiologist can help you save money on the cost of your hearing healthcare and ensure that you receive the best possible care within the guidelines of your insurance plan.
What are hearing aid benefit administrators in the hearing care industry?
In the hearing care industry, a third-party hearing aid benefit administrator refers to organizations or entities that are separate from the patient and the healthcare provider but are responsible for reimbursing or paying for the services rendered. These third-party payers may include insurance companies, government programs, employers, or other organizations that provide health coverage or benefits.
How Do They Work With Providers?
Providers in the hearing care industry, like American Hearing & Audiology, often need to establish contracts or agreements with these hearing aid benefit administrators to be considered in-network and receive reimbursement for the services they provide. To best serve our patients, we went through that process and have become an in-network provider for all major insurance carriers and their affiliated hearing aid benefit administrators.
- Provider Contracting: TPAs often enter into contracts or agreements with hearing care providers to establish a network of in-network providers. The contracts define the terms and conditions for reimbursement, including rates, billing procedures, and any specific requirements for participating in the network. Hearing care providers who agree to the contract become part of the TPA’s network and may be listed in the provider directories.
- Claims Submission and Reimbursement: Hearing care providers submit claims to the TPA for services rendered to patients covered by the TPA’s healthcare plans. The TPA reviews the claims for accuracy, eligibility, and adherence to the plan’s guidelines. Once the claims are approved, the TPA reimburses the hearing care provider according to the agreed-upon reimbursement rates and payment schedules.
What type of hearing aids do hearing aid benefit administrators cover?
TPA Coverage
The coverage provided by Hearing Aid Benefit Administrators, aka Third-Party Administrators (TPAs) can vary depending on the specific TPA and the insurance plan they administer.
Insurance plans administered by TPAs may offer coverage for different types of hearing aids based on the terms of the plan and the specific policies chosen by the employer or organization. Coverage may include a range of hearing aid styles, technologies, and brands. Some insurance plans may have specific criteria for coverage, such as the degree of hearing loss, the need for medical necessity documentation, or preferred (in-network) providers that must be used.
Since we participate with the major TPAs, including but not limited to, United Healthcare, Nations Hearing, and TruHearing, our specialists are able to maximize your savings while providing unparalleled hearing care.
When do benefits reset?
The frequency with which you can get new hearing aids with insurance coverage can vary depending on the specific insurance plan or policy, but they typically reset every 1 to 3 years. Fortunately, this allows patients to benefit from recent hearing aid advancements at regular intervals. You’d be amazed at how often new features are released as the technology improves. For some folks, the same hearing aids might meet their needs for 4+ years, but that doesn’t mean they’re getting as much out of their devices as they could with pairs released more recently. As the technology develops, so do the ways in which hearing instruments can improve a user’s life, and that’s not something to miss out on.
How American Hearing + Audiology Helps
When you’re a patient with us, our staff will help you maximize your benefits by verifying the frequency at which you can receive new technology, and they’ll help you remember when your benefits renew so that you can enjoy the latest technology for little to no out-of-pocket cost. If you have any questions, please give us a call!
Does Medicare cover hearing aids?
While Medicare (Traditional) does not typically include hearing aid benefits, Medicare Advantage now includes benefits that can provide you with advanced hearing aids at little to no out-of-pocket cost. If you have Medicare Advantage and are in need of hearing loss treatment, give your nearest American Hearing location a call today!
What is the difference between Medicare and Medicare Advantage?
- Medicare: Medicare is a federal health insurance program primarily for individuals aged 65 and older, as well as certain younger people with disabilities. It consists of several parts: – Medicare Part A: This covers hospital insurance, including inpatient hospital stays, skilled nursing facility care, hospice care, and some home healthcare services. Most people do not pay a premium for Part A if they or their spouse have paid Medicare taxes while working.
– Medicare Part D: This provides prescription drug coverage, which can be obtained through standalone Part D plans or Medicare Advantage plans that include prescription drug coverage. Part D plans are offered by private insurance companies, and premiums and coverage vary.
- Medicare Advantage (Medicare Part C): Medicare Advantage plans are an alternative way to receive Medicare benefits. Offered by private insurance companies approved by Medicare, these plans must provide at least the same level of coverage as Original Medicare (Parts A and B). However, they can also offer additional benefits not covered by Original Medicare, such as dental, vision, hearing, and fitness programs. Medicare Advantage plans typically require individuals to use a network of healthcare providers, but don’t worry, because we are!
Do other hearing centers participate in Medicare Advantage?
Many DO NOT. WE DO!
- We participate with EVERY insurance plan in our area, including Medicare Advantage, where other hearing practices are out of network. Make American Hearing + Audiology your FIRST STOP for IN-NETWORK hearing aid benefits!
- If a hearing center cannot confirm that they are in-network with Medicare Advantage, you won’t be able to save nearly as much as if they were.
Many hearing centers don’t partner with Medicare Advantage. However, American Hearing covers participants regardless of their plans.
Medicare Advantage plans have a network of providers offering services at lower costs to members. American Hearing + Audiology agrees to these rates, lowering your expenses. Visiting an out-of-network center could mean higher costs and different coverage rules.
Review your Medicare Advantage plan for hearing service coverage, as coverage varies. Medicare offers limited hearing aid coverage, so a Medicare Advantage plan can provide additional benefits.
In short, savings are less likely at centers not in-network with Medicare Advantage. For peace of mind, contact American Hearing & Audiology, which is in-network with Medicare Advantage.
What has changed in how hearing aid benefits are handled?
Recent Changes
Over the last five years, the hearing care industry has changed dramatically. Previously, you and your insurance company would combine to pay a higher, “bundled price” for hearing aids that included unlimited ongoing service and support for a period of 3 to 5 or more years. As recently as 2017, we estimate that only 20-35% of patients had hearing aid insurance benefits to pay a portion of the cost of hearing aids.
Now, it works a bit differently. First the GOOD NEWS – we estimate that 60-75% of patients with hearing loss have some type of hearing aid benefit due to the addition of hearing aid benefits to most Medicare Advantage insurance plans. BUT, today’s hearing aid benefits are DIFFERENT than before. Today, these benefits help pay for the electronics, a hearing test, programming and delivery of the hearing aids plus a limited number of follow-up appointments. They do not cover the cost of ongoing service and support that patients need to maintain their hearing aids and keep you hearing your best (professional cleaning, routine adjustments, etc.). Click below to learn about how you can continue to save on additional follow-up appointments and more.
